Vaccines and Antiviral Drugs for Treatment
In some cases, vaccines can be used to treat an active viral infection. The concept behind this is that by giving the vaccine, immunity is boosted without adding more disease-causing virus. In the case of rabies, a fatal neurological disease transmitted via the saliva of rabies virus-infected animals, the progression of the disease from the time of the animal bite to the time it enters the central nervous system may be two weeks or longer. This is enough time to vaccinate individuals who suspect that they have been bitten by a rabid animal, and their boosted immune response is sufficient to prevent the virus from entering nervous tissue. Thus, the potentially fatal neurological consequences of the disease are averted, and the individual only has to recover from the infected bite. This approach is also being used for the treatment of Ebola, one of the fastest and most deadly viruses on Earth. Transmitted by bats and great apes, this disease can cause death in 70 to 90 percent of infected humans within two weeks. Using newly developed vaccines that boost the immune response in this way, there is hope that affected individuals will be better able to control the virus, potentially saving a greater percentage of infected persons from a rapid and very painful death.
Another way of treating viral infections is the use of antiviral drugs. Because viruses use the resources of the host cell for replication and the production of new virus proteins, it is difficult to block their activities without damaging the host. However, we do have some effective antiviral drugs, such as those used to treat HIV and influenza. Some antiviral drugs are specific for a particular virus and others have been used to control and reduce symptoms for a wide variety of viral diseases. For most viruses, these drugs can inhibit the virus by blocking the actions of one or more of its proteins. It is important to note that the targeted proteins be encoded by viral genes and that these molecules are not present in a healthy host cell. In this way, viral growth is inhibited without damaging the host.
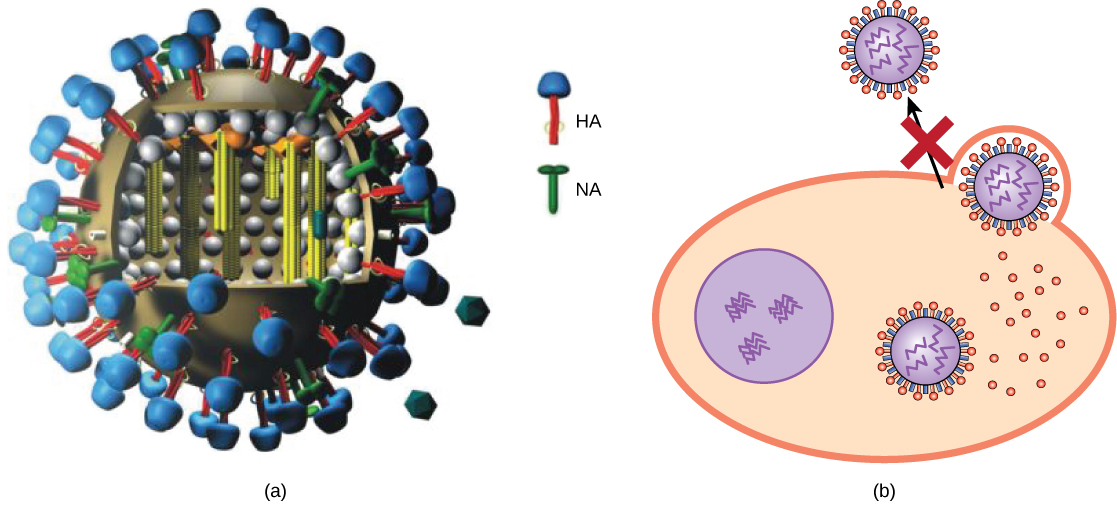
Antivirals have been developed to treat genital herpes (herpes simplex II) and influenza. For genital herpes, drugs such as acyclovir can reduce the number and duration of episodes of active viral disease, during which patients develop viral lesions in their skin cells. As the virus remains latent in nervous tissue of the body for life, this drug is not curative but can make the symptoms of the disease more manageable. For influenza, drugs like Tamiflu (oseltamivir) (Figure) can reduce the duration of “flu” symptoms by one or two days, but the drug does not prevent symptoms entirely. Tamiflu works by inhibiting an enzyme (viral neuraminidase) that allows new virions to leave their infected cells. Thus, Tamiflu inhibits the spread of virus from infected to uninfected cells. Other antiviral drugs, such as Ribavirin, have been used to treat a variety of viral infections, although its mechanism of action against certain viruses remains unclear.
By far, the most successful use of antivirals has been in the treatment of the retrovirus HIV, which causes a disease that, if untreated, is usually fatal within 10 to 12 years after infection. Anti-HIV drugs have been able to control viral replication to the point that individuals receiving these drugs survive for a significantly longer time than the untreated.
Anti-HIV drugs inhibit viral replication at many different phases of the HIV replicative cycle (Figure). Drugs have been developed that inhibit the fusion of the HIV viral envelope with the plasma membrane of the host cell (fusion inhibitors), the conversion of its RNA genome into double-stranded DNA (reverse transcriptase inhibitors, like AZT), the integration of the viral DNA into the host genome (integrase inhibitors), and the processing of viral proteins (protease inhibitors).
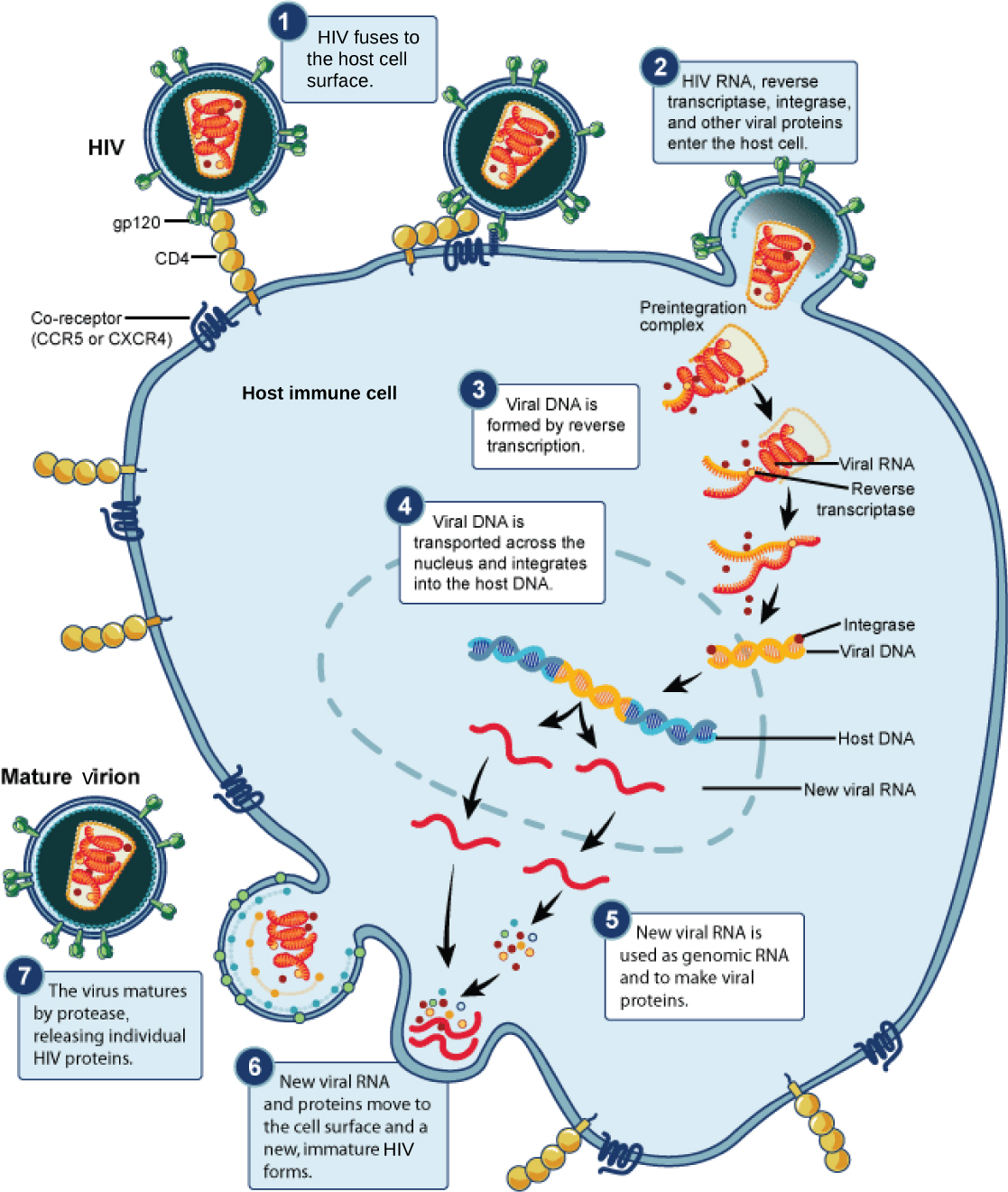
Unfortunately, when any of these drugs are used individually, the high mutation rate of the virus allows it to easily and rapidly develop resistance to the drug, limiting the drug’s effectiveness. The breakthrough in the treatment of HIV was the development of HAART, highly active anti-retroviral therapy, which involves a mixture of different drugs, sometimes called a drug “cocktail.” By attacking the virus at different stages of its replicative cycle, it is much more difficult for the virus to develop resistance to multiple drugs at the same time. Still, even with the use of combination HAART therapy, there is concern that, over time, the virus will develop resistance to this therapy. Thus, new anti-HIV drugs are constantly being developed with the hope of continuing the battle against this highly fatal virus.
Everyday Connection
Applied Virology:
The study of viruses has led to the development of a variety of new ways to treat non-viral diseases. Viruses have been used in gene therapy. Gene therapy is used to treat genetic diseases such as severe combined immunodeficiency (SCID), a heritable, recessive disease in which children are born with severely compromised immune systems. One common type of SCID is due to the lack of an enzyme, adenosine deaminase (ADA), which breaks down purine bases. To treat this disease by gene therapy, bone marrow cells are taken from a SCID patient and the ADA gene is inserted. This is where viruses come in, and their use relies on their ability to penetrate living cells and bring genes in with them. Viruses such as adenovirus, an upper-respiratory human virus, are modified by the addition of the ADA gene, and the virus then transports this gene into the cell. The modified cells, now capable of making ADA, are then given back to the patients in the hope of curing them. Gene therapy using viruses as carriers of genes (viral vectors), although still experimental, holds promise for the treatment of many genetic diseases. Still, many technological problems need to be solved for this approach to be a viable method for treating genetic disease.
Another medical use for viruses relies on their specificity and ability to kill the cells they infect. Oncolytic viruses are engineered in the laboratory specifically to attack and kill cancer cells. A genetically modified adenovirus known as H101 has been used since 2005 in clinical trials in China to treat head and neck cancers. The results have been promising, with a greater short-term response rate to the combination of chemotherapy and viral therapy than to chemotherapy treatment alone. This ongoing research may herald the beginning of a new age of cancer therapy, where viruses are engineered to find and specifically kill cancer cells, regardless of where in the body they may have spread.
A third use of viruses in medicine relies on their specificity and involves using bacteriophages in the treatment of bacterial infections. Bacterial diseases have been treated with antibiotics since the 1940s. However, over time, many bacteria have evolved resistance to antibiotics. A good example is methicillin-resistant Staphylococcus aureus (MRSA, pronounced “mersa”), an infection commonly acquired in hospitals. This bacterium is resistant to a variety of antibiotics, making it difficult to treat. The use of bacteriophages specific for such bacteria would bypass their resistance to antibiotics and specifically kill them. Although phage therapy is in use in the Republic of Georgia to treat antibiotic-resistant bacteria, its use to treat human diseases has not been approved in most countries. However, the safety of the treatment was confirmed in the United States when the U.S. Food and Drug Administration approved spraying meats with bacteriophages to destroy the food pathogen Listeria. As more and more antibiotic-resistant strains of bacteria evolve, the use of bacteriophages might be a potential solution to the problem, and the development of phage therapy is of much interest to researchers worldwide.